
A bunion, medically termed hallux valgus, is a bony protrusion on the inner side of the foot, precisely at the base of the big toe. This condition arises from the misalignment of the bones in the forefoot, compelling the big toe to angle towards the lesser toes, consequently protruding the joint at its base. Bunions can cause significant discomfort and interfere with your daily activities. If you have exhausted nonsurgical options like padding or orthotic shoes, bunion surgery may be the next step to relieve your pain and improve mobility. During the procedure, a podiatrist may remove the bunion, realign bones, or release tight ligaments to straighten your big toe. Risks of bunion surgery include nerve damage, bone healing issues, or overcorrection. The recovery process often takes up to six months. Initially, you may need to keep your leg elevated to reduce swelling, and it can take weeks before you can comfortably wear regular shoes again. Among the long-term benefits of bunion surgery are improved comfort and mobility. If you are struggling with bunion pain, it is suggested that you consult a podiatrist to discuss whether surgery is right for you.
If you are suffering from bunions, contact Dr. Richard DiMario of Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
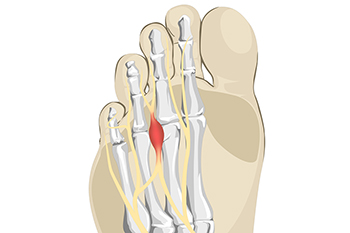
Morton's neuroma, named after the American surgeon Thomas G. Morton who first described it in the 19th century, is a painful condition affecting the nerves in the foot. This benign growth typically forms between the third and fourth toes, resulting from compression or irritation of the interdigital nerve. The exact cause of Morton's neuroma remains elusive, but factors such as wearing tight or high-heeled shoes, engaging in repetitive high-impact activities, or foot deformities may contribute to its development. Symptoms of Morton's neuroma often include a sharp, burning pain or sensation of a lump or foreign object in the ball of the foot. Individuals may also experience numbness, tingling, or a feeling of walking on a pebble. As the condition progresses, discomfort may worsen and become more persistent, particularly during weight-bearing activities. If you have pain in this part of your foot, it may be Morton's neuroma, and it is suggested that you visit a podiatrist. This type of doctor can accurately diagnose and effectively treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Richard DiMario of Maine. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

When it comes to walking versus running, the distinction goes beyond just pace and intensity. As experts note, the mechanics of each activity necessitate specific footwear for walking and running. For walkers, shoes with soft, flexible soles are recommended to absorb the impact of each step and facilitate the rolling motion from heel to toe. Runners require thicker-soled shoes for ample shock absorption, given the varied striking points on the foot during a run. It is important to remember that while running shoes can serve for walking, the reverse is not recommended by experts. Footwear plays a critical role in preventing foot injuries like plantar fasciitis and Achilles tendonitis, but shoes alone cannot resolve existing issues. Seeking guidance from a podiatrist is essential if foot discomfort persists. To ensure the right shoe fit, have your arch and gait evaluated. For advice with foot pain related to either walking or running, it is suggested that you schedule an appointment with a podiatrist for a full exam and diagnosis. The appropriate treatment options will follow, including suggestions on the right type footwear for the activity.
For more information about walking shoes versus running shoes, consult with Dr. Richard DiMario from Maine. Our doctor can measure your feet to determine what your needs are and help you find an appropriate pair of footwear.
Foot Health: The Differences between Walking & Running Shoes
There are great ways to stay in shape: running and walking are two great exercises to a healthy lifestyle. It is important to know that running shoes and walking shoes are not interchangeable. There is a key difference on how the feet hit the ground when someone is running or walking. This is why one should be aware that a shoe is designed differently for each activity.
You may be asking yourself what the real differences are between walking and running shoes and the answers may shock you.
Differences
Walking doesn’t involve as much stress or impact on the feet as running does. However, this doesn’t mean that you should be any less prepared. When you’re walking, you land on your heels and have your foot roll forward. This rolling motion requires additional support to the feet.
Flexibility – Walking shoes are designed to have soft, flexible soles. This allows the walker to push off easily with each step.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Custom orthotics, often associated with runners or athletes, offer benefits beyond the realm of sports. These specialized shoe inserts are designed to address imbalances in foot structure, which can significantly impact posture and overall body alignment. Even a minor imbalance can lead to problems throughout the body. Orthotics may be beneficial if you notice uneven wear on the soles of your shoes or have frequent ankle sprains. Chronic pain in the heels, misaligned toes, or abnormal foot positioning during walking are other reasons that orthotics may be needed. By providing support and stability, orthotics help distribute weight more evenly across the foot, reducing strain on muscles and joints. They can correct biomechanical issues, improve gait efficiency, and alleviate discomfort associated with various conditions. Whether you are an athlete or someone seeking relief from everyday discomfort, custom orthotics offer a simple yet effective solution to enhance foot function and promote overall well-being. If you are interested in learning more about how custom-made orthotics can help you, it is suggested that you consult a podiatrist.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Foot pain caused by arthritis can be debilitating, affecting mobility and quality of life. Arthritis in the feet often presents with symptoms such as joint stiffness, swelling, tenderness, and reduced range of motion. This pain may worsen with activity and improve with rest, making it challenging to engage in daily tasks comfortably. Different types of arthritis can affect the feet, including osteoarthritis, rheumatoid arthritis, and gout. Osteoarthritis typically develops due to wear and tear on the joints over time, while rheumatoid arthritis is an autoimmune condition that affects the lining of the joints. Gout results from the accumulation of uric acid crystals in the joints. If you have foot pain that persists or worsens, especially if accompanied by other symptoms like swelling or warmth in the joints, it is suggested that you schedule an appointment with a podiatrist for an accurate diagnosis and treatment. If the pain is determined to be arthritic, a podiatrist can offer relief methods to help maintain mobility and enhance your quality of life.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Richard DiMario from Maine. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.

Rheumatoid arthritis, or RA, a chronic autoimmune condition, can have a profound effect on the feet, causing pain, swelling, and stiffness that significantly impair mobility and quality of life. In RA, the immune system mistakenly attacks the lining of the joints, many of which are in the feet, leading to inflammation and joint damage. Common symptoms of RA in the feet include tender, swollen joints, particularly in the toes and ankles, and difficulty walking or bearing weight due to pain and stiffness. Over time, untreated RA can cause deformities such as bunions, hammertoes, or flat feet, further compromising foot function and comfort. Additionally, RA can increase the risk of other foot problems, such as corns, calluses, or ulcers, particularly if mobility is limited or proper foot care is neglected. If you are afflicted by this condition, it is suggested that you are under the care of a podiatrist who can accurately diagnose RA and provide you with a comprehensive management plan.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Richard DiMario of Maine. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.

Cuboid syndrome is a lesser-known condition that affects the cuboid bone, one of the seven tarsal bones located in the midfoot. This syndrome occurs when the ligaments surrounding the cuboid bone become strained or injured, leading to pain and discomfort along the outer side of the foot. Cuboid syndrome is often misunderstood or misdiagnosed, due to its symptoms overlapping with other foot ailments such as ankle sprains or stress fractures. The characteristic symptoms of cuboid syndrome include pain, tenderness, and swelling on the lateral aspect of the foot, particularly during weight-bearing activities like walking or running. The pain may also worsen with certain movements, such as pushing off the ground or standing on tiptoes. Understanding the distinct features of cuboid syndrome and its diagnostic criteria are essential for accurate identification and appropriate management. If you have pain in the outside part of your foot, it is suggested that you promptly schedule an appointment with a podiatrist for an exam, a diagnosis, and suggested treatment options.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with Dr. Richard DiMario from Maine. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our office located in York, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.

Calcaneal spurs, also known as heel spurs, are bony protrusions that form on the underside of the heel bone, which is the calcaneus. These spurs develop in response to long-term inflammation and tension on the plantar fascia, a band of tissue that connects the heel bone to the toes. The repetitive stress and strain can lead to the formation of calcium deposits, resulting in the development of bony growth. Individuals with calcaneal spurs often experience symptoms such as sharp pain in the heel, particularly during weight-bearing activities like walking or standing. The pain may intensify with the first steps in the morning or after prolonged periods of rest. Additionally, tenderness and swelling around the affected area are common. While some people with calcaneal spurs may not experience any symptoms, others may find the pain debilitating, impacting their daily activities. If you have heel pain, it is strongly suggested that you visit a podiatrist who can accurately diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. Richard DiMario from Maine. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in York, ME . We offer the latest in diagnostic and treatment technology to meet your needs.